Code Blue is a stressful situation especially if you are not well aware of the patient before. Here I attempted to make any Code Blue easy.
Below are sequence of steps that happen during a Code Blue. They can vary depending on several factors.
Patient unresponsive, not breathing or gasping and/or pulseless.
Make sure to Check Code status of the patient
Call the operator for ‘Code Blue’ announcement. There is a button for this in the patient’s room on the wall. Operator announces overhead.
Systematic approach to assess and treat a patient in Cardiac arrest involves
1. BLS assessment [(1). Check responsiveness by tapping and shouting, “Are you all right?” (2). Check for carotid Pulse and breathing (3). Activate the emergency response system and obtain an AED. (4) Defibrillation]
2. Primary assessment [ ABCDE. (A) Airway, (B) Breathing, (C) Circulation, (D) Disability, (E) Expose.]
3. Secondary assessment [SAMPLE. (S) Signs and symptoms; (A) Allergies; (M)Medications; (P)Past Illnesses; (L)Last Oral Intake; (E) Events Leading Up To Present Illness., 5 Hs and 5 Ts]
Focus on two things:
1. Start high-quality CPR (one- and two-person rescuer) at a rate of 100-120 compressions per minute, at least 2 inches (5 cm) deep and 30:2 compressions-ventilation ratio for adults, minimize interruptions to compressions to less than 10sec.
Head Tilt-Chin Lift to open the airway. Put the mask on the face and give each breath for one sec to see visible chest rise and give an other breath after one sec.
Use E-C clamp technique to hold the bag-mask device in the hospital.
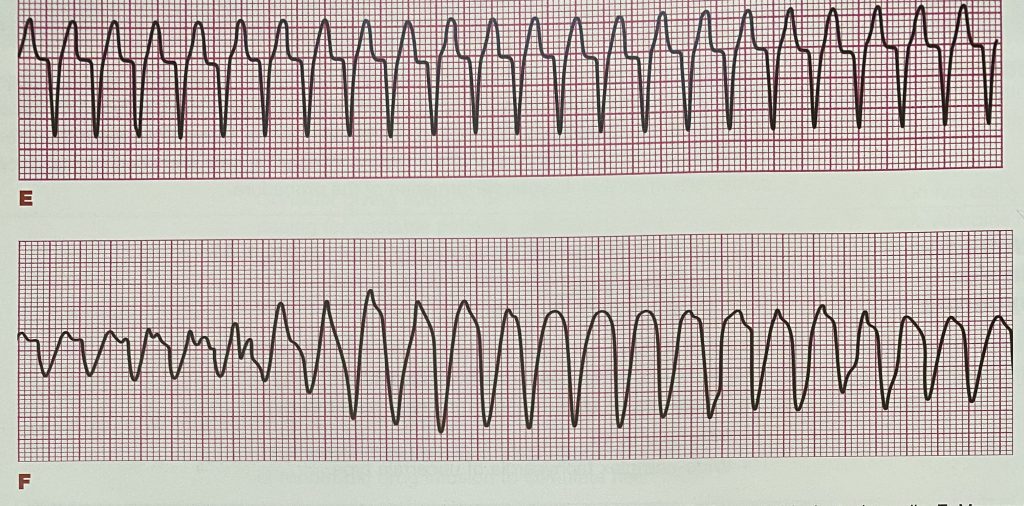
2. Rapid defibrillation for “shockable rhythms-pulseless ventricular tachycardia and ventricular fibrillation. AED helps with this.

All the code team arrives into the patient’s room in couple of minutes-Hospitalist, floor RN, ICU RN, Respiratory therapist, security, etc.
Review “Adult Cardiac Arrest Algorithm“.
Examine the patient quickly. Check for JVD, mental status, pupils, lung sounds, heart sounds, pedal edema, pallor specifically apart from complete physical exam.
Ask the RN the AM labs, patient’s diagnosis and other pertinent information about the patient. Review the chart in the computer by yourself if needed while code is going on.
Hospitalist can order some STAT labs [especially if no recent blood work done] like CBC, CMP, Cardiac Enzyme-TN T, ABG, etc.
Think of 5Hs and 5Ts as part of SECONDARY assessment along with . I put in colors to remember easily.
>Hypovolemia [low volume]: Hypotension resulting from bleeding or excessive diuresis. Give IVF-NS bolus 1L at least.
>Hypoxia [low Oxygen]: ABG stat which may show respiratory acidosis. Usually; CHF or COPD. Fluid overload due to excessive iv fluids-Give IV Lasix. May need intubation.
>Hydrogen ions [Acidosis =high H+]: Can give Na Bicarbonate IV.
>Hypo [low Potassium]or Hyperkalemia [high Potassium ]: Review AM labs to show if this is the issue.
>Hypothermia [low Temp]: rare to encounter this as a hospitalist in hospital. Bear hugger to raise the core temp.
>Tension Pneumothorax [Pressure on lungs]: Tracheal deviation. Unequal breath sounds on right and left.
>Tamponade, Cardiac [Pressure on heart]: Tachycardia, JVD, feeble pulse etc. Needs Pericardiocentesis. Call Cardiac surgery immediately.
>Toxins: Usually for ER docs. Drugs usually are TCA, B blockers, CCBs, Digoxin.
>Thrombosis, Pulmonary: PE [Blood clots in lungs]: Get stat CTA chest if suspecting PE after stabilizing the patient. Start IV Heparin.
>Thrombosis, Coronary [Blood clots in coronaries]: MI: Cardiology stat. May need to go to cath lab once stabilized.
Hospitalist runs the code.
Nurses bring crash cart or code cart-contains emergency medications and equipment, such as a monitor/defibrillator or AED and airway adjunct, arrange bag mask device, oxygen, attach EKG leads, attach defibrillation pads, administer medications, set up for potential intubation, set up Continuous Waveform Capnography, coordinate compressions etc, arrange a bed in ICU.
Attach Automated External Defibrillator (AED) [ A monophasic defibrillator is generally set to deliver 360J for defibrillation, and a biphasic defibrillator is initially set to deliver between 120 and 200 J] to check the rhythm.
Do not place pads over medicine patches or devices like PPM or ICD.
Shave the chest if too much hair is present.
AED may show Shockable or Non Shockable rhythm. If non Shockable, continue compressions. If shockable, give shock.
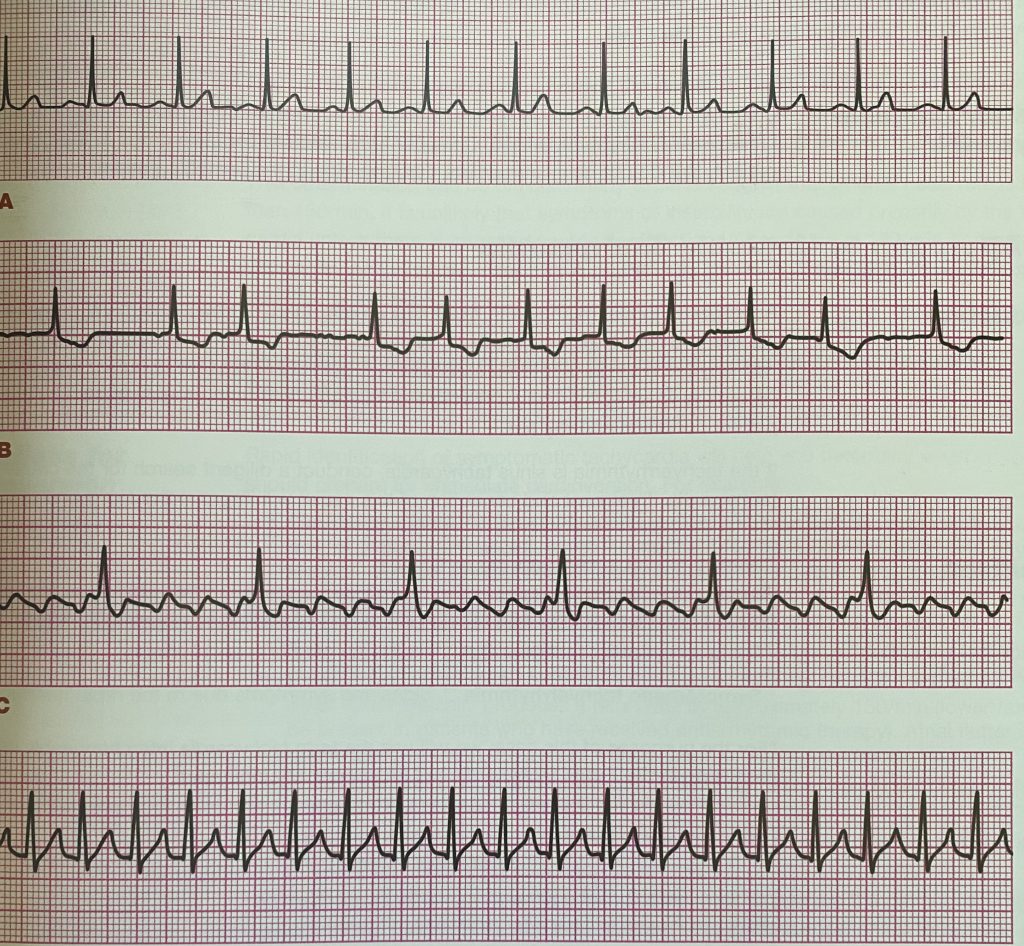
Synchronized Cardioversion: Increasing dose with each subsequent shock
SVT, Atrial Flutter: 50J–> 75J–> 100J
VTac : 100J–>150J–>200J [note that it’s double the energy than SVT and Aflutter]
AFib: 120J–>150J–>200J [same as VTac except the starting dose]
Switch compressor roles approximately every 2 minutes (or after about 5 cycles of compressions and ventilations at a ratio of 30:2)
CPR/Back board to be placed for compressions when available.
Use Feedback device to monitor the quality of CPR.
Continuous waveform capnography monitors adequacy of CPR [If PETCO2 <10mm Hg, improve CPR] and if ROSC returned [Abrupt sustained increase in PETCO2 >40mm Hg].
“Closed loop” communication between health care workers
As soon as the shock is delivered, resume chest compressions immediately even if a normal heart rhythm is seen, give 2 minute CPR
If the patient is intubated and code needs to continue, CPR should be done continuously and give breaths once every 6 seconds for all ages.
Results of ACLS code:
>Patient may not get ROSC. Check for return of spontaneous circulation (ROSC) by checking the carotid pulse.
>If the patient attains ROSC, Follow ADULT IMMEDIATE POST-CARDIAC ARREST CARE ALGORITHM. RR at 10bpm, Target PETCO2 of 35-40mm Hg, Maintain Oxygen saturation >=94%, IV fluids-NS or LR 1-2Liters. I remember this algorithm by the pneumonic “REND” if the patient requires an I.V. vasopressor for Hypotension maintain a systolic BP of at least 90 mm Hg. R=ROSC,
E=Epinephrine infusion 2-10 mcg/min,
N=NorEpinephrine infusion 0.1-0.5 mcg/kg/min,
D=Dopamine infusion 5-20 mcg/kg/min.
Patient goes to ICU.
>If the physician is unable to intubate the patient, the operator may page an anesthesiologist to intubate the patient
>If the arrest was due to cardiac causes, the patient may be taken to the cardiac catheterization lab (if the facility has one) or to the ICU.
>Targeted Temperature Management [Therapeutic hypothermia] after transferring to ICU may be considered for patients with ROSC who are unresponsive for next 24hrs.
>If the patient has Bradycardia [but has pulse] causing Hypotension, Altered mental status or chest discomfort or CHF, Follow ADULT BRADYCARDIA WITH A PULSE ALGORITHM. I remember this algorithm by the pneumonic “BADE“. B=Bradycardia HR<50, A=Atropine 0.5mg every 3-5min; max of 3mg, D=Dopamine infusion 2-20mcg/kg/min, E=Epinephrine infusion 2-10mcg/min.
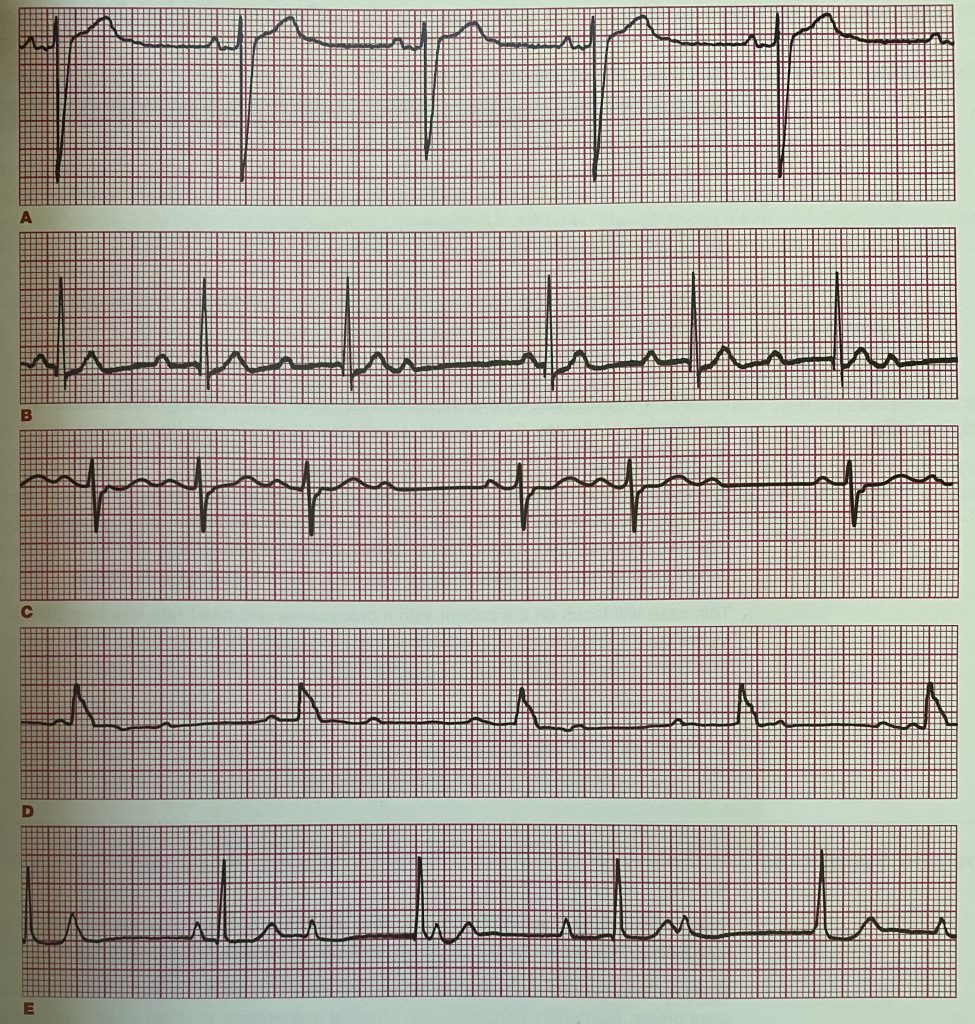
Some Indications for Pacing in Bradycardia: AED [pic above] can do transcutaneous pacing [TCP]. Severe Hypothermia is a contraindication for pacing.
-Unstable Bradycardia. Unstable during a code means patient has hypotension, acutely altered mental status, signs of shock, ischemic chest discomfort, or acute heart failure.
-Mobitz type 2 second degree heart block
-Third degree heart block
>If the patient has Tachycardia, causing Hypotension, Altered mental status or chest discomfort or CHF, follow ADULT TACHYCARDIA WITH A PULSE ALGORITHM. I remember this algorithm by the pneumonic “TaPAS“. Ta=Tachycardia, P=Procainamide start at 20-50mg/min; maintenance infusion at 1-4mg/min, A=Amiodarone 150mg first iv in 10min; maintenance infusion at 1mg/min for 6 hrs, S=Sotalol 100mg over 5 min.
High Performance Team Dynamics: Code team should follow the following rules.
Clear roles and responsibilities
Knowing your limitations
Knowledge sharing
Summarizing & Reevaluating
Closed-Loop communication
Clear messages
Mutual respect.
What to do with Younger Patients:
[In the case of Code for a child from 1 yr of age to puberty, you can just one hand to do CPR if the child is small. If unwitnessed collapse in this age group, first give 2 minutes of CPR before activating Emergency Response System. Compressions should be 1/3rd of chest diameter and about 2 inches. If there is no breathing but has pulse, give rescue breaths every 3-5 seconds. Compression-Ventilation ratio: 30:2 with one rescuer and 15:2 with two rescuers.]
[For infants less than one year of age, pulse checked in the inside of the upper arm. Compressions should be 1/3rd of chest diameter and about 1.5 inches. For Chest compressions, use 2 fingers with one rescuer and 2 thumbs with 2 rescuers. CPR for HR <60/min. Compression-Ventilation ratio: 30:2 with one rescuer and 15:2 with two rescuers. Do not tilt or extend neck beyond neutral position.]
How to get ACLS/BLS certifications online?
![]()

